
Symptomatic treatment of hyperglycaemia, aim for blood glucose level 19.7 mmol/L) and hyperbilirubinaemia (>342 μmol/L), and detection of carbamyl-haemoglobin in patients with uraemia can all falsely elevate HbA1c. Major comorbidities likely to limit life expectancy Severe hypoglycaemia or hypoglycaemia unawareness Requiring any antidiabetic agent other than metformin or insulinĭiabetes of longer duration or clinical cardiovascular disease Australian Diabetes Society position statement on recommended glycated haemoglobin (HbA1c) targets 9ĭiabetes of short duration and no clinical cardiovascular disease Guidance on HbA1c targets is detailed in the Australian Diabetes Society (ADS) recommendations (Table 2). HbA1c targets should be individualised for each patient on the basis of their type of diabetes, life expectancy, risk of hypoglycaemia, duration of disease and other comorbidities. 9 Thus, while achieving HbA1c targets should form the focus of diabetes management, this needs to be weighed against the risks of intensive therapy.
#Hemoglobin a1c normal range in pregnancy trial#
9 Higher rates of hypoglycaemia were evident in trial arms with intensive glycaemic control, and particular caution should be exercised in older patients, those with near-normal glycaemic control or those with a higher risk of cardiovascular disease. Microvascular rather than macrovascular events are reduced with tight glycaemic control in more established disease. Tight glycaemic control appears to provide greater benefit if implemented early in the disease process when compared with implementation at a more advanced disease stage.
The UKPDS demonstrated that achieving an HbA1c of 53 mmol/mol (7.0%) with intensive therapy using insulin or sulfonylurea (in comparison to 63 mmol/mol in the conventional arm) led to a 25% risk reduction in microvascular, but not macrovascular, outcomes. 8 However, the risk of severe hypoglycaemia increased with lower HbA1c values. 7,8 The DCCT showed that intensive insulin therapy leading to HbA1c of 53 mmol/mol (7.0%, in comparison to 77 mmol/mol in the conventional arm) reduced the risk of retinopathy, nephropathy and neuropathy by 35–70%. The Diabetes Chronic Complications Trial (DCCT) and United Kingdom Prospective Diabetes Study (UKPDS) were two landmark trials that unequivocally demonstrated the benefit of glycaemic control for delaying and reducing the rate of end-organ complications in type 1 and type 2 diabetes, respectively. Iron/erythropoietin-stimulating agent administration Causes of falsely low or high glycated haemoglobin (HbA1c) 10,5,27Ĭhange in red blood cell lifespan or turnover However, it is limited by various conditions affecting its accuracy (Table 1), greater cost and low sensitivity. Advantages of measuring HbA1c for this purpose include its convenience without a need for pre-test preparation, sample stability when collected and less day-to-day variability. It should be measured in individuals at risk of diabetes. HbA1c ≥48 mmol/mol (≥6.5%) in a laboratory using a validated method is diagnostic of diabetes. 6 As a result of the continuous turnover of erythrocytes, it is estimated that only 50% of an HbA1c value represents glucose exposure in the preceding 30 days, while 40% represents exposure in the previous 31–90 days and 10% in the previous 91–120 days. 4 As the mean erythrocyte lifespan is approximately 120 days, HbA1c acts as a surrogate marker of glucose concentration during the preceding 8–12 weeks. HbA1c is dependent on the interaction between the concentration of blood glucose and the lifespan of the erythrocyte. 4 HbA1c results from the covalent attachment of glucose to the N-terminal valine of the haemoglobin β-chain in a nonenzymatic process known as glycation. 4,5 Within HbA, approximately 6% is glycated, of which the main component is HbA1c (5%), with minor components of HbA1a and HbA1b (1%).

Normal adult haemoglobin (HbA) comprises a haem moiety and two globin chains, the α and β chains (α2β2), making up approximately 97% of adult haemoglobin. Haemoglobin is the iron-containing oxygen-transport protein present in erythrocytes.

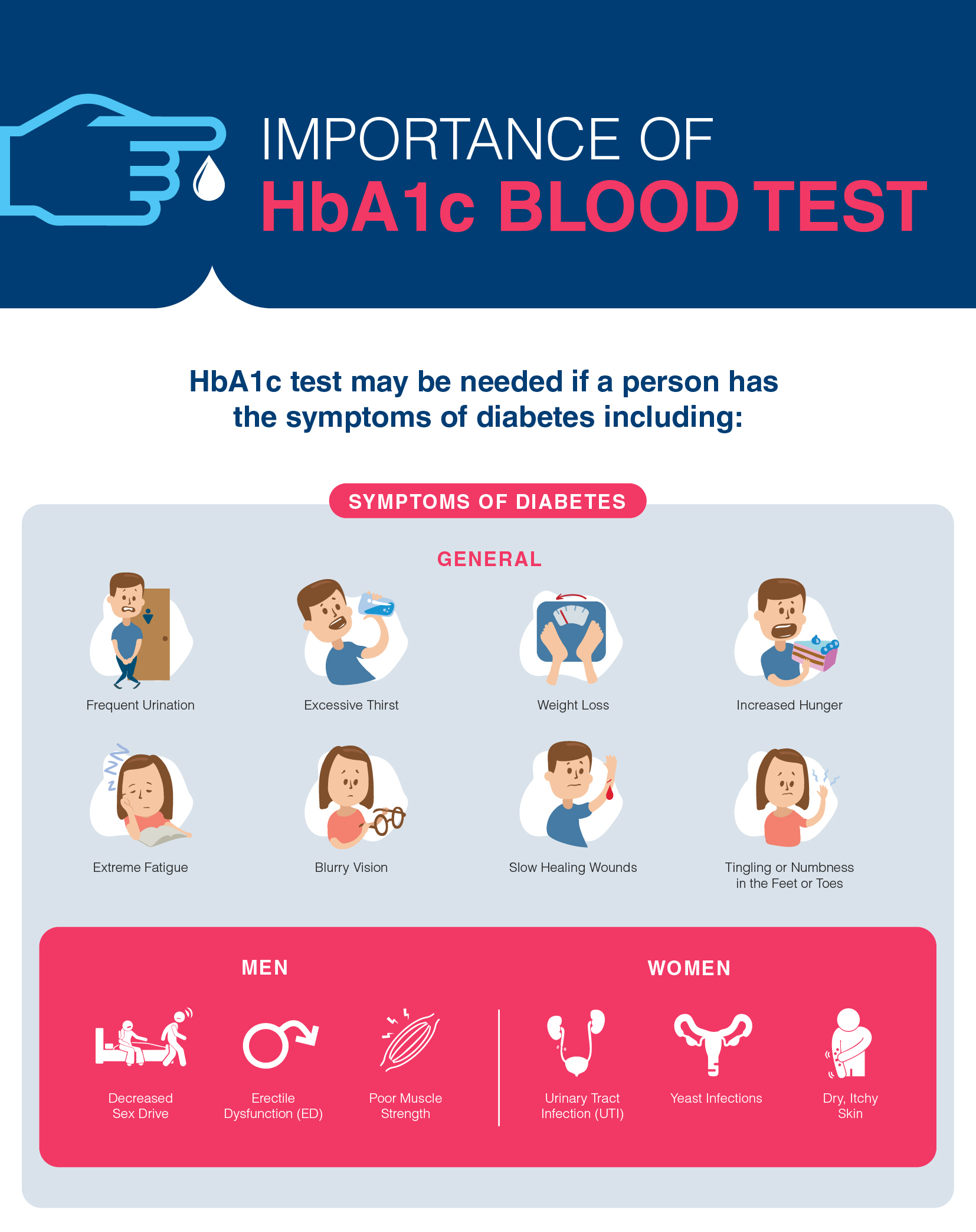
2 The HbA1c test is listed on the Medicare Benefits Schedule (MBS) for subsidy once every 12 months for the diagnosis of diabetes (HbA1c ≥48 mmol/mol ) in high-risk individuals, and up to four times per year for monitoring of established diabetes. HbA1c was initially not endorsed for the diagnosis of diabetes however, assay improvements led to the ADA validating its use in 2010 as a diagnostic criterion for diabetes at a cutoff of ≥6.5%, pre-diabetes between 5.7% and 6.4%, and normal <5.7%. 1 For decades, the diagnosis of diabetes relied on glucose criteria through using either fasting glucose, random glucose or the 75 g oral glucose tolerance test (OGTT). The use of glycated haemoglobin, or HbA1c, has become the standard of assessing glycaemic control in patients with diabetes since the American Diabetes Association (ADA) recommended its use in 1988.


 0 kommentar(er)
0 kommentar(er)
